Abstract
BACKGROUND: Microvascular and arterial thromboses are well described in patients with thrombotic microangiopathy (TMA) including complement mediated TMA (CM-TMA)/atypical hemolytic uremic syndrome. Hemolytic disorders are associated with increased risk of venous thromboembolism (VTE), and patients with CM-TMA may have additional risk factors of hospitalization and central lines and may not consistently receive thromboprophylaxis due to thrombocytopenia. However, little is known about the prevalence and clinical correlates of VTE in CM-TMA.
METHODS: We performed this single center retrospective cohort study of consecutive patients with CM-TMA enrolled in the Johns Hopkins Complement Associated Disease Registry between January 2014 and December 2020. Data regarding clinical presentation, laboratory studies including clinical complement gene sequencing, terminal complement inhibition and anticoagulation therapy, VTE events including characteristics and risk factors for VTE were collected. A diagnosis of CM-TMA was based on: (1) platelet count <150 × 10 9/L, (2) schistocytes on peripheral blood smear or TMA on renal biopsy, if performed, (3) ADAMTS13 activity >10%, (4) Shiga toxin negative, and (5) serum creatinine >2.25 mg/dL at presentation, which was considered supportive but not required for diagnosis. We only included VTE events post-CM-TMA diagnosis. VTE characteristics, treatment and outcomes were summarized using descriptive statistics. The Chi-squared test and Mann Whitney test were used to compare categorical and continuous variables across groups with and without VTE, respectively.
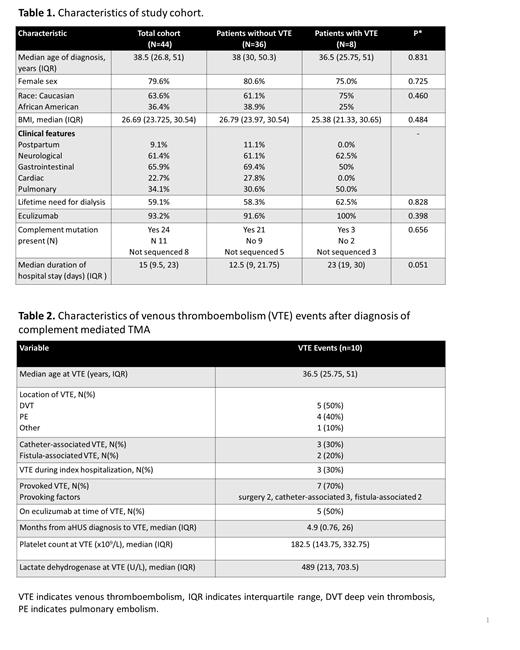
RESULTS: Of 44 patients diagnosed with CM-TMA and followed for a median of 3.1 years (IQR 0.8-5.5), 8 (18.2%) experienced at total of 10 VTE events (5.6 VTE events/100 patient-years). There was no significant difference between patients with and without VTE in age at diagnosis, sex, race, BMI, need for dialysis, treatment with eculizumab, and presence of mutations in complement genes (Table 1).
VTE events included 5 deep vein thromboses, 4 pulmonary emboli and 1 splenic infarct (Table 2). The majority (70%) of VTE events were provoked with 5 (50%) associated with a catheter or vascular access for dialysis and 2 (20%) events following major surgeries. The median time from CM-TMA diagnosis to the first VTE event was 4.9 months (IQR 0.76-26) with 3 events occurring during the index hospitalization for CM-TMA. Of 10 VTE events, 5 occurred while on complement inhibition and 2 on anticoagulation (1 on therapeutic and 1 on prophylactic anticoagulation). Of note, only 1 of 3 patients diagnosed with VTE during their index CM-TMA hospitalization received thromboprophylaxis. At the time of VTE diagnosis, the median platelet count was 182.5 x 10 9/L (IQR 143.75-332.75); 80% had a platelet count >150 x 10 9/L , and 10% each had a platelet count <50 x 10 9/L or 50-150 x 10 9/L.
VTE was treated with therapeutic anticoagulation with enoxaparin, warfarin or a direct oral anticoagulant in 7 of 8 patients for a median duration of 7 months (IQR 4-14). One patient experienced recurrent PEs; the first PE occurred 2 months following the index CM-TMA hospitalization and the second event was 4 years later while off of anticoagulation and complement inhibition. A second patient experienced a splenic infarct 7 months after initial CM-TMA diagnosis while non-compliant with ravulizumab, followed by a catheter-associated upper extremity DVT 2 months later while on therapeutic anticoagulation and ravulizumab. No VTEs were fatal.
CONCLUSION: VTE is common in patients with CM-TMA (18.2%), with a prevalence comparable to thrombotic thrombocytopenic purpura (18%, Tse et al. 2020) but greater than that reported in dialysis patients (Moinar et al. 2017). In CM-TMA patients, VTE is commonly provoked by hospitalization or dialysis catheters and tends to occur after platelet count recovery and in the absence of thromboprophylaxis. Factors such as renal impairment, prolonged hospitalization, complement dysregulation, and free hemoglobin release may also increase VTE risk. Our results highlight the high prevalence of VTE in CM-TMA and the importance of thromboprophylaxis once the platelet count is greater than 50 x 10 9/L.
Dane: Alexion: Honoraria; Sanofi Genzyme: Honoraria; Janssen: Honoraria. Chaturvedi: Sanofi Genzyme: Other: Advisory board member; Alexion: Other: Advisory board member; Dova: Other: Advisory board member; Argenx: Other: Advisory board member; UCB: Other: Advisory board participation.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal